Review of Article:
Peripheral Vascular Hemodynamics
Review and commentary by Jon Miles,
Miles Research
“Peripheral
Vascular Hemodynamics in the Bulbar Conjunctiva of
Subjects with Hypertensive Vascular Disease” by Richard E. Lee and Elizabeth A.
Holze
(From the
Department of Medicine, The
Journal of
Clinical Investigation 1951, pp. 539-546. [J Clin
Invest. 1951 Jun;30(6):539-46 ]
For a copy
of the original study:
www.milesresearch.com/pdf/hemodynamics.pdf
For more
references to related studies on conjunctival vessels
and microangiopathy:
www.milesresearch.com/main/References-ConjunctivalVessels.asp
Online source of this document:
www.milesresearch.com/main/hemodynamics.asp
Introduction
This
research into peripheral vascular reactivity, carried out with only the basic
technologies available 55 years ago, is a landmark study of conjunctival
vascular hemodynamics. In this study, the vasculature
of the bulbar conjunctiva is subject to a number of examinations, including
description and measurement of vessel geometry and morphology, measurements of
peripheral blood flow, and response to both topical epinephrine and cold pack.
In this
review, the methods and results are summarized with additional commentary and
interpretation.
Based on
quantitative microscopic observations, the study compares the structure and
behavior of conjunctival vasculature among patients
with and without hypertension and other disorders.
Subjects
were classified into one of three groups:
Group I: Normotensive
without known disease (N=72)
Group II: Hypertensive with vascular disease
(N=45)
Group III: Normotensive
with various diseases (N=33)
Comparison
of the results from Groups I and II illustrates the effect of hypertension and
vascular disease on microvessel structure and
function. Comparison of results from Group III with those from Group I
illustrate the effect of non-hypertensive diseases on the microvessels.
Group III was included to show how the amount of random variability in
characteristics present among subjects with non-hypertensive disease is
relatively high in comparison to the consistent pattern of responses found
among the hypertensive subjects.
Detailed
examination of the structure and behavior of the conjunctival
microvasculature can be useful in detecting incipient pathology, and with
recently available camera and
photogrammetric pattern recognition
technology, the method can be automated and applied to digital eye images for
screening hypertension risk.
Background
Peripheral
vascular reactivity can be monitored via microscopic examination in studies of
functional aspects of muscular vessels in the capillary bed of living mammals.
In prior studies, comparison of several hemodynamic
disturbances (such as hypertension, acute hemorrhage, prolonged hypotension)
showed that each separate condition had a distinctive characteristic status
reflected in the capillary bed of the mesentery.
In animal
studies, it has been observed that the mesenteric vascular bed in experimental
renal hypertension was predominantly constricted, with ischemic arterioles and
capillaries, and a similar elevation of epinephrine response, along with
hyperplasia of vascular elements. No single feature was found pathognomic or characteristic of any of the experimental
syndromes, however the combination of indicators considered together found
among the hypertensive group was found to be consistently characteristic.
Methods
Observations
of the conjunctival vessels among subjects in each of
the three groups included both qualitative and quantitative evaluations of the
structure and function of the vessels, as well as the vascular response to
locally applied epinephrine and cold packs.
First the
state of the capillary bed was noted, including conditions such as ischemic,
plethoric, euvascular, vessel tortuosity
was graded, and spontaneous vasomotor activity in the precapillary
sphincter was graded.
Second, the
velocity of blood flow was measured in metarterioles,
capillaries, and collecting venules. Measurement was
made by observing the vessels at 47X, and recording the transit time of blood
cells across a relatively straight segment of length 70 to 100 microns.
Third,
spontaneous vasomotor activity was measured in terms of responsiveness to
applied stimuli. Vasomotion is an apparently
spontaneous variation in caliber resulting from contraction and relaxation of
the vascular smooth muscle. The vasomotor reactivity of the vessels to
topically applied epinephrine and cold pack was graded in terms of amount of
stimulation required to elicit threshold vasoconstriction. The sensitivity to
topical epinephrine was graded by applying increasing concentrations at
3-minute intervals, starting with 1:800,000 and increasing, until
vasoconstriction is observed. Vasoconstriction response to cold was measured by
applying an ice pack to the closed eyelid for increasing-length intervals until
constriction is observed.
Subjects
The group
of normotensive non-diseased subjects included 72
subjects with no known disease.
The group
of hypertensive subjects included 14 men and 31 women (average age 31, ranging
from 3 to 78). Blood pressure in this group was consistently greater than
140/100 in all subjects.
The group
of normotensive with disease included 33 patients
having such disorders as multiple myeloma, cirrhosis,
peptic ulcer, polycythemia, and psychosomatic
conditions. None of this group had any history of hypertension.
Some of the
studies, such as measurements of peripheral blood flow, were conducted on a
subset of the population, 10 cases from each group.
Results
Peripheral Vascular Findings
General Nature of the Vascular
System
|
Group I Normotensive with no disease (N=72) |
Group II Hypertensive
with vascular disease (N=45) |
Group III Normotensive with various disease (N=33) |
|
Vessels
tonic; flow smooth and rapid; no stagnation |
Vessels
narrowed; tissue ischemic; flow slowed |
Variable,
from wide dilation and sluggish flow, to euvascular |
Summary:
- in the normotensive
non-disease group: the vessels are tonic with good flow (euvascular).
- in the hypertensive person: vessels are narrowed and tissue is
ischemic with deficiency of vessels, and reduced flow.
- in the normotensive
with disease group: variable, ranging from normal to abnormal, with no
pattern.
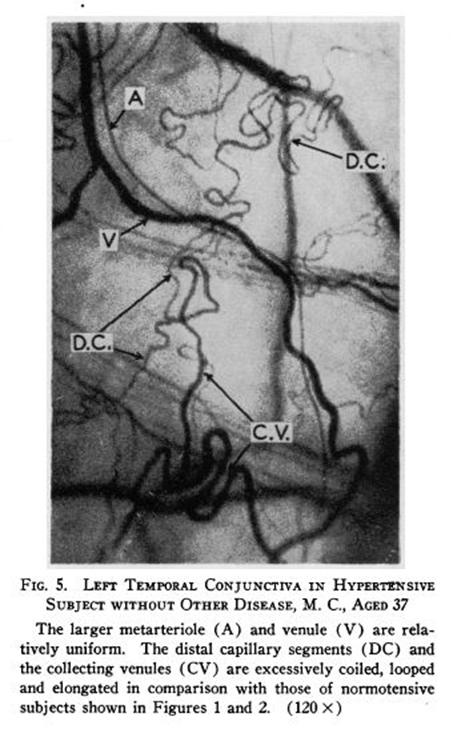
Hypertension
is associated with reduced blood flow and vessel narrowing. Example vessel
topography is illustrated in the figures.
Coiling, Tortuosity,
Looping of Vessels
|
Group I Normotensive with no disease (N=72) |
Group II Hypertensive
with vascular disease (N=45) |
Group III Normotensive with various disease (N=33) |
|
Up to
grade 1 in 8% of cases |
Grade 3
to 4 in 62% of cases; grade 1 to 2 in 12% of cases |
Up to
grade 1 in 18% of cases |
Summary:
- in the normotensive
non-disease group: the vessels are mostly non-tortuous, with only 8%
graded as high as 1.
- in the hypertensive person: vessels are significantly tortuous with
grade 3 to 4 found in about 2/3 of cases.
- in the normotensive
with disease group: slightly more vessel tortuosity
than normal cases..
Clearly,
vessel tortuosity is associated with hypertension.
Velocity of Peripheral Blood Flow
|
Cell Velocity in microns/sec |
Group I Normotensive with no disease (N=10) |
Group II Hypertensive
with vascular disease (N=10) |
Group III Normotensive with various disease (N=10) |
|||
|
|
Mean |
S.E. |
Mean |
S.E. |
Mean |
S.E. |
|
End
Arterioles |
110 |
30 |
23 |
4 |
34 |
10 |
|
Capillaries |
26 |
2 |
10 |
1 |
8 |
4 |
|
Venules |
56 |
5 |
18 |
1 |
16 |
6 |
Hypertensive
cases had blood cell velocities that were lower than the normotensive
blood cell velocity in all three segments of the conjunctival
microvasculature. Among the hypertensive, all with blood pressures over
140/100, blood cell velocity in the end arterioles were 21% of normal; in the
capillaries 38% of normal, and in the collecting venules
32% of normal.
Among the hypertensive
cases, the blood cell velocity was 1/3 to 1/5 found in the control group in all
three segments of the microvasculature. Among the normotensive
non-disease cases, blood cells had a velocity in the collecting venules that was 51% the rate observed in the end
arterioles, whereas the hypertensive group cell velocity in the collecting venules is 78% of the velocity in the arterioles. This
suggests that causal factors of the impaired circulation in hypertension are in
the arterial segments.
The blood
circulation in hypertensive patients is under high pressure with reduced
velocity. The heart is working hard to push the blood through the arterial
tree, but is meeting considerable resistance to the flow, and despite pumping
under high pressure, the flow is reduced.
Spontaneous Vasomotor Activity at Precapillary Sphincters
|
Group I Normotensive with no disease (N=12) |
Group II Hypertensive
with vascular disease (N=15) |
Group III Normotensive with various disease (N=12) |
|
Present
up to grade 1 in 3 of 12 cases; variable in duration and frequency |
Grade 3-4
in 11 of 15 cases; rapid; closed phase predominated |
Not
usually seen, highly variable |
As Lee and Holze write, “In both normotensive
and hypertensive subjects vasomotion varied in rate
and duration of the dilated and the constricted phases. In the hypertensive, in
contrast to findings in all other subjects, it [the vasomotion]
was more rapid with relatively long periods of precapillary
narrowing. This resulted in intermittent, or interrupted, capillary blood flow.
A sudden jet-like column of red cells would enter the capillary and flow would
be uniform for several seconds. The stream was then gradually reduced as the precapillary narrowed, with subsequent longer periods
during which only scattered red cells were admitted into the capillary from the
parent arteriole.”
In the normotensive non-disease group, the spontaneous vasomotor
activity is present only to a limited extent, and in only 25% of subjects. In
the hypertensive group, spontaneous vasomotor activity is elevated, with the
closed phase dominant. In the normotensive with
disease group, spontaneous vasomotor activity was usually not seen, but when
found was variable, ranging from normal to abnormal, with no pattern.
The
hypertensive cases showed hyperactivity of the precapillary
sphincter vasomotion, but with impaired flow.
Epinephrine Sensitivity
(Concentration
required to produce threshold pre-capillary and metarteriolar narrowing)
|
Group I Normotensive with no disease (N=12) |
Group II Hypertensive
with vascular disease (N=15) |
Group III Normotensive with various disease (N=12) |
|
Mean:
1:37,000 S.E.:
1:3,760 Range:
1:20,000 to 1:50,000 |
Mean:
1:298,000 S.E.:
1:24,700 Range: 1:100,000
to 1:800,000 |
Mean:
1:314,000 S.E.:
1:32,000 Range:
1:10,000 to 1:800,000 |
In the normotensive non-disease group, the concentration of
epinephrine needed to produce vasoconstriction was an order of magnitude less
than that required for the hypertensive group. Among hypertension subjects,
sensitivity to topical epinephrine was observed to be 10 times greater than the
normotensive subjects. Among the normotensive
with disease cases, sensitivity was variable, ranging from normal to abnormal,
with no pattern. This group was elevated above Group I (Normotensive
non-disease) only in Laennec’s cirrhosis and hyperglobulinemia.
Hypertensive
cases were significantly more sensitive to topical epinephrine than the control
group.
Cold Reactivity
Vasoconstriction
Reaction to Cold Ice Pack Application
|
Group I Normotensive with no disease (N=n/a) |
Group II Hypertensive
with vascular disease (N=27) |
Group III Normotensive with various disease (N=21) |
|
No
reaction among any of those tested |
Grade 1:
7 cases; Grade 2: 1 case |
Variable,
grades 0 thru 4 |
In the normotensive non-disease group, there was no observable
effect of cold application to vasoconstriction, whereas the hypertensive group
had about one third responding to cold. In the normotensive
with disease group, Vasoconstriction reaction to cold was found to be variable,
ranging from normal to abnormal, with no pattern. Patients with hyperglobulinemia in this group responded with grade 4
vasoconstriction, stagnant flow, and red cell aggregates.
Hypertensive
cases were significantly more sensitive to the topical application of a cold
pack than the control group.
Conclusion
From
consideration of all the measurements and differences between hypertensive
patients and controls in the structure and behavior of the conjunctival
microvasculature, it is clear that hypertension is related to impaired blood
flow, vessel narrowing, and vasomotor hypersensitivity. Among the hypertensive
patients, the heart is working harder than normal to push blood cells through
the arteriolar tree, but is meeting with elevated resistance, resulting in
impaired blood flow. The cause of the higher flow resistance appears to be
vessel narrowing. Among these patients, not only is the peripheral circulation
reduced, the microvessels are hypersensitive to
constricting factors.
The study
shows that high blood pressure is a result of not simply ‘arteries clogged with
lipids’ but abnormal vascular topography and abnormal vasomotor sensitivity.
The
observational methods used in this study include measurements of structural and
behavioral properties of the conjunctival vasculature.
With current generation cameras and image processing techniques, the clinician
can record these images and subject them to automated analysis to assess risk
factors for hypertension.
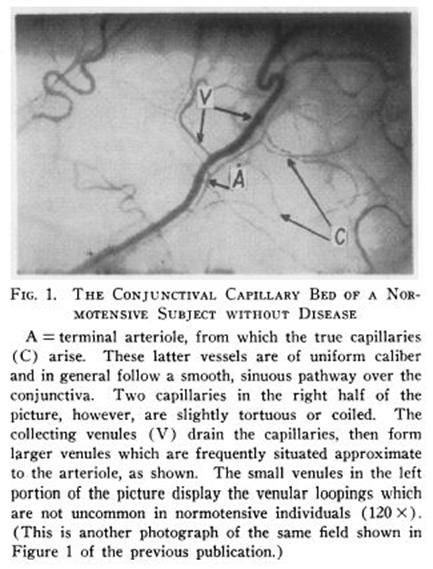
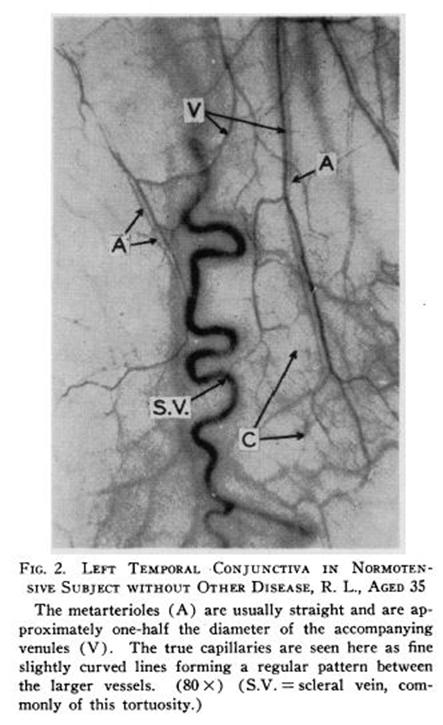
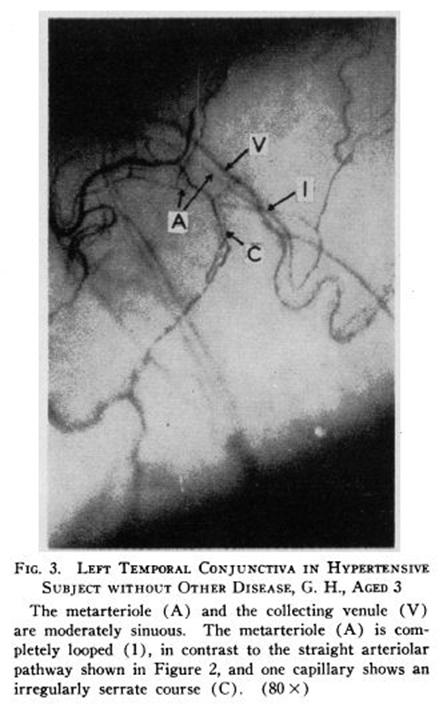
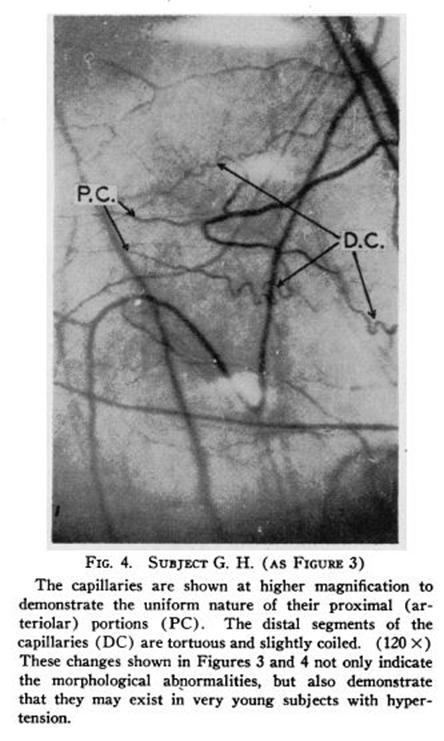
Sample Photographs of Conjunctival Vessels